What is Radiofrequency Ablation?


Benefits
Effective Pain Relief
Long-Lasting Results
Minimally Invasive
Quick Recovery
Improves Mobility
Reduction in Medications
Outpatient Procedure
Low Risk of Complications
Expanded Guide
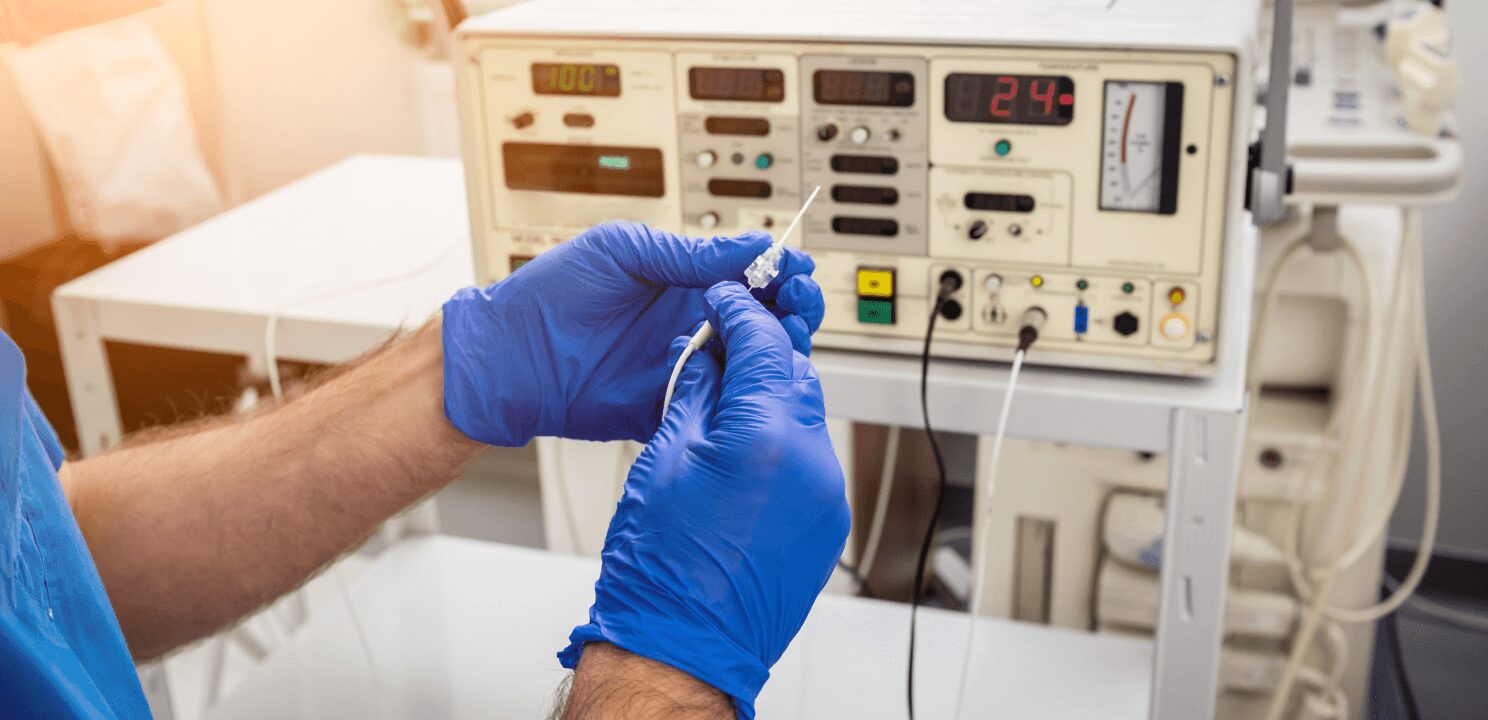
Radiofrequency ablation (RFA) is a minimally invasive procedure that provides long-lasting relief from chronic pain by using heat generated from radiofrequency energy to disrupt pain-carrying nerves. This procedure is especially beneficial for patients with chronic back, neck, and joint pain due to conditions such as spondylosis (spinal arthritis) and sacroiliac joint pain. There are two main types of RFA used to target specific pain sources: thermal RFA and Lateral Branch Neurotomy. Both methods are used to interrupt pain signals from nerves, but each targets different areas and types of pain.
Thermal Radiofrequency Ablation (RFA)
Thermal RFA is a common approach for treating chronic pain in the spine, especially for patients with spondylosis. Spondylosis is a degenerative condition where spinal discs and facet joints experience wear and tear, often leading to pain, stiffness, and reduced mobility. In thermal RFA, a physician uses imaging guidance, such as fluoroscopy, to precisely position a thin probe near the nerves that supply the painful facet joints. Once the probe is correctly placed, radiofrequency energy heats the surrounding nerve tissue to a temperature that “ablates” or destroys the nerve, stopping it from transmitting pain signals. This process is carefully controlled to ensure that only the targeted nerves are affected, preserving function in surrounding tissues.
The procedure takes about 30 to 60 minutes and is typically performed on an outpatient basis under local anesthesia, allowing patients to go home the same day. Studies show that 70-80% of patients experience significant pain relief following thermal RFA, with many reporting a 50% or greater reduction in pain that can last six months to a year or longer. Thermal RFA is particularly useful for individuals with spondylosis who have not found sufficient relief from conservative treatments like medications, physical therapy, or facet joint injections.
Lateral Branch Neurotomy
Lateral Branch Neurotomy is a specialized form of RFA focused on alleviating pain from the sacroiliac (SI) joints, which connect the spine to the pelvis. Sacroiliac joint pain is often caused by arthritis, injury, or inflammation and can lead to significant discomfort in the lower back, buttocks, and legs. The lateral branches of the sacral nerves supply the SI joints, and Lateral Branch Neurotomy targets these branches to reduce pain.
During the procedure, similar to thermal RFA, a physician uses imaging guidance to position a small probe near the lateral branch nerves. Radiofrequency energy is then applied to disrupt the pain-carrying nerves, preventing them from transmitting pain signals from the SI joint area. This procedure also takes around 30 to 60 minutes and is typically performed on an outpatient basis, allowing patients to go home afterward. Studies indicate that Lateral Branch Neurotomy can provide significant pain relief for SI joint pain, with results lasting from several months to over a year. Many patients report improved mobility and reduced pain that allows them to resume daily activities comfortably.
Indications for Radiofrequency Ablation
Radiofrequency ablation is indicated for individuals with chronic pain conditions like spondylosis and sacroiliac joint pain who have not found adequate relief through conservative treatments such as medications, physical therapy, or steroid injections. Patients with spondylosis often suffer from neck or lower back pain due to arthritic changes in the spine, while those with sacroiliac joint pain may experience lower back and pelvic discomfort that radiates down the legs. RFA can provide targeted relief for these conditions by focusing on the specific nerves responsible for pain in the affected areas.
Benefits
Radiofrequency ablation (RFA) offers numerous benefits for managing chronic pain, particularly in patients with back, neck, and joint issues. One of the primary advantages is effective, targeted pain relief, as RFA disrupts the nerves responsible for transmitting pain signals, often reducing pain by 50% or more. This relief is long-lasting, with results typically lasting from six months to a year and, in some cases, even longer. The procedure is minimally invasive, requiring only a small needle and no open surgery, which reduces tissue disruption and allows for a quick recovery. Most patients can return to normal activities within a few days, as RFA is an outpatient procedure with minimal downtime. By alleviating pain, RFA also improves mobility, enabling patients to engage in daily activities more comfortably. Many patients find they can reduce or eliminate long-term pain medications, lowering the risk of side effects and dependency. With a complication rate of less than 1%, RFA is considered a safe, effective option, particularly for those who cannot undergo more invasive treatments. These combined benefits make RFA a valuable solution for those seeking durable relief from chronic pain.
Conclusion
Radiofrequency ablation, encompassing both thermal RFA and Lateral Branch Neurotomy, is an effective and minimally invasive treatment option for chronic pain conditions such as spondylosis and sacroiliac joint pain. By selectively targeting pain-carrying nerves, RFA provides lasting relief and enables patients to resume daily activities with greater comfort. With high success rates, a low complication profile, and the potential to improve quality of life, RFA is a valuable option for patients who seek to manage their pain without the need for invasive surgery.
Frequently Asked Questions
Have more questions? Schedule a consultation with Dr. Patel to gain additional insights and discuss treatment options. We are committed to advancing your health through patient education and a safe, minimally invasive approach.
Gramercy Center
Take the first step towards a healthier life by scheduling your initial consultation with Dr. Patel. At our clinic, we specialize in minimally invasive procedures that offer faster recovery, improved function, and decreased pain. Our client-centered approach ensures that you receive the highest quality care tailored to your unique needs. We look forward to offering you an exceptional experience.